Your risk of recurrence
All people who have had breast cancer have a personal risk of recurrence, and yours is unique to you.
It looks like you are using an older version of Internet Explorer which is not supported. We advise that you update your browser to the latest version of Microsoft Edge, or consider using other browsers such as Chrome, Firefox or Safari.
Keep Ahead has been developed and funded by Novartis Pharmaceuticals UK Limited. This site is intended for UK early breast cancer patients and general public.
All people who have had breast cancer have a personal risk of recurrence, and yours is unique to you.
After facing breast cancer, the thought of the cancer returning can be difficult to come to terms with. It is important to remember that most breast cancers do not return after treatment.
You should have regular conversations with your doctor about your personal risk of recurrence and whether adjuvant therapy is a suitable option for you. You can take steps to help reduce the risk of your cancer returning and increase your chances of a cancer-free future.
Most cancers do not come back after treatment.15 However, there is a chance that breast cancer may come back months or years after the initial diagnosis and treatment. It is called breast cancer recurrence.
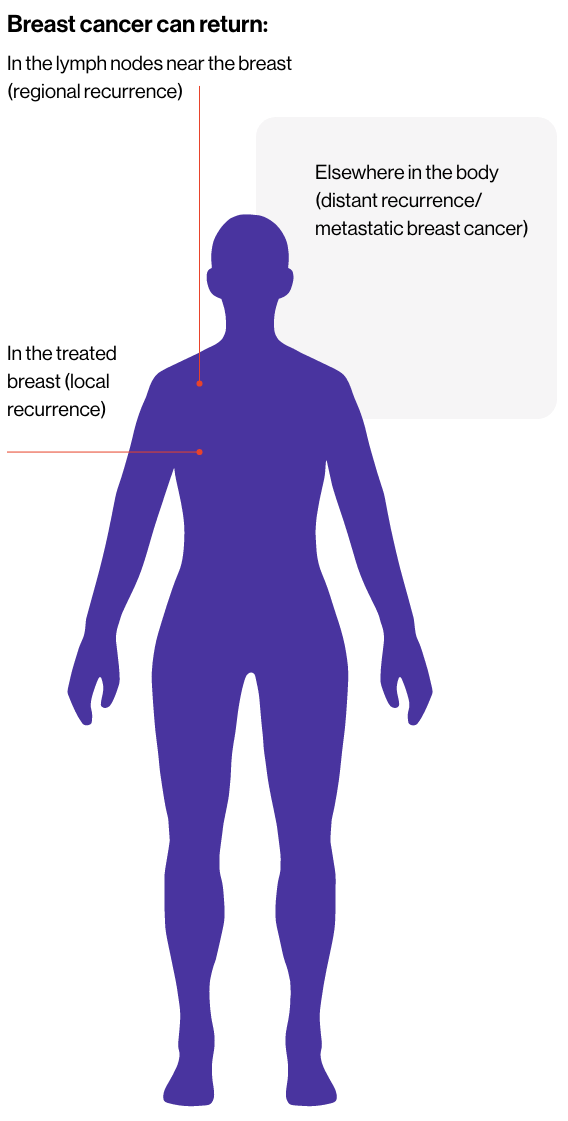
Recurrence is when the cancer returns after initial treatment with surgery, chemotherapy, immunotherapy and/or radiotherapy. The type of recurrence depends on where the cancer comes back:
Rarely a new, unrelated tumour may form in your opposite or treated breast. This would not be classed as a breast cancer recurrence, rather a new, primary cancer.11 Most cancers do not come back after treatment. However, after surgery and other initial treatments a few individual cancer cells may remain in the body and may start to grow again, causing cancer recurrence.2
Because of this risk of recurrence after surgery and other initial therapies, you may be prescribed further treatments to reduce the risk of breast cancer coming back and decrease the risk of progression to metastatic breast cancer14 which currently cannot be cured but can often be controlled or managed for extended periods.

Just as no two cancer journeys are the same, the risk of recurrence varies between each person. Your risk depends on many factors, including the specific type of breast cancer you had, how advanced it was, and the treatments you received.1 It is important to remember that every breast cancer patient has some degree of risk, so make sure you understand your individual risk by having this discussion with your Healthcare professional.
There are several factors that can influence the likelihood of breast cancer returning. Knowing what they are can help you have open conversations with your healthcare team about your specific situation:

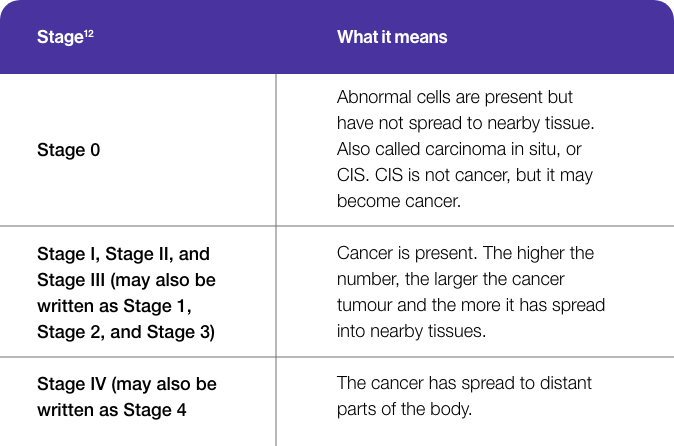
There are different staging systems that help to describe the stage of breast cancer. The most commonly used in the UK is the TNM score. TNM stands for Tumour, Node, Metastasis and measures tumour size, presence of metastasis and if there is cancer present in your lymph nodes.9
Sometimes patients & doctors may describe the diagnosis using the term 'stages'. Generally, the higher the stage, the greater the risk of recurrence.22
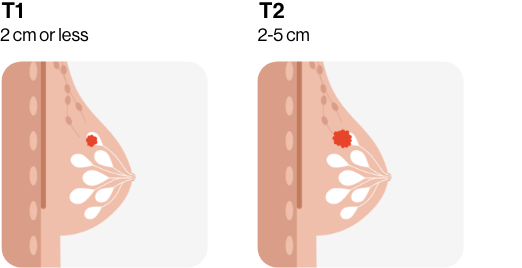
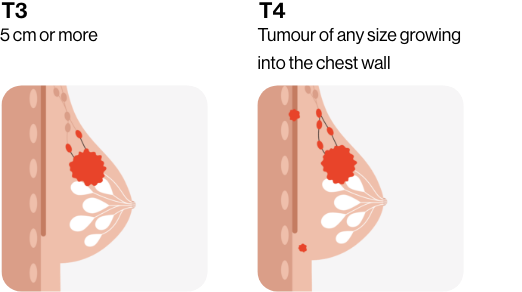
Larger cancers often have a higher risk of recurrence than smaller cancers. You might hear your multidisciplinary team (MDT) speak about T1, T2, T3 and T4, which refers to the size and/or extent of the main tumour.12
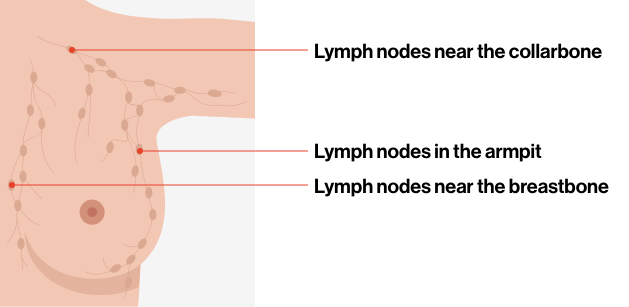
If cancer was found in the lymph nodes, the risk of recurrence may be higher. This is why lymph nodes are often carefully monitored during treatment. The more ‘positive’ lymph nodes, the higher the risk of recurrence.13
Your MDT might speak about N numbers.
N0: There is no cancer in nearby lymph nodes. N1, N2, N3: Refers to the number and location of lymph nodes that contain cancer. The higher the number after the N, the more lymph nodes that contain cancer.13
Together with your T numbers and N numbers, your healthcare professionals are able to better understand the severity of your breast cancer. To learn more about TNM staging, visit the terminology page.
Patients with N0 but other high-risk features present are at higher risk of recurrence than those without high-risk features.10
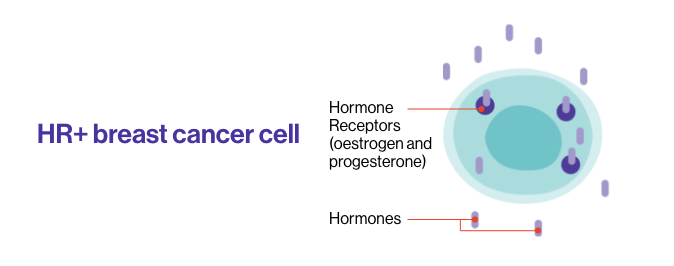
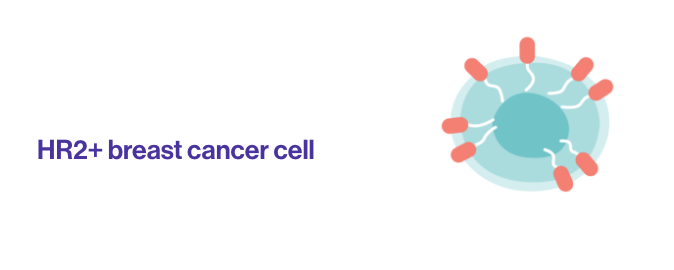
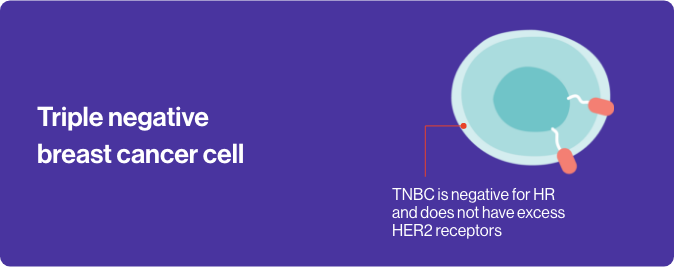
Tumour markers are proteins that can be used to define the subtype of cancer that you have and help your doctor to decide on what treatment is best for you.
In breast cancer, testing for 3 Tumour Markers is routinely performed on every tumour: oestrogen receptor, progesterone receptor and human epidermal growth factor receptor 2 (HER2) status.
Different subtypes of breast cancer have different risk of recurrence. ROR in the first 5 years is higher with triple negative and HER2+ tumours.
Whilst the ER+/HER2- subtype has lower risk or recurrence overall, it remains elevated for a longer time.
The type of treatment you received, whether surgery, chemotherapy, radiotherapy, immunotherapy, targeted therapy and/or hormone therapy can impact risk of recurrence. Following your treatment plan closely can reduce the likelihood of cancer returning. Speak to your cancer team for more information.1
Treatments may cause side effects. If you are struggling to take your treatment for any reason, please speak to your doctor or nurse. There are different ways to help ease the side effects, to find out more please visit the Royal Marsden website here.


A person's age at the time of breast cancer diagnosis can influence the chances of the cancer returning. This is due to several factors, including how the body changes over time and how breast cancer behaves and responds to treatment at different ages.1, 21.
Women diagnosed with hormone receptor-positive, HER2-negative breast cancer at a younger age, especially under 35, have a higher chance of their cancer returning compared to women in their 40s. This may be because younger women tend to have more aggressive tumours that are more likely to recur, regardless of the specific treatment approach.20
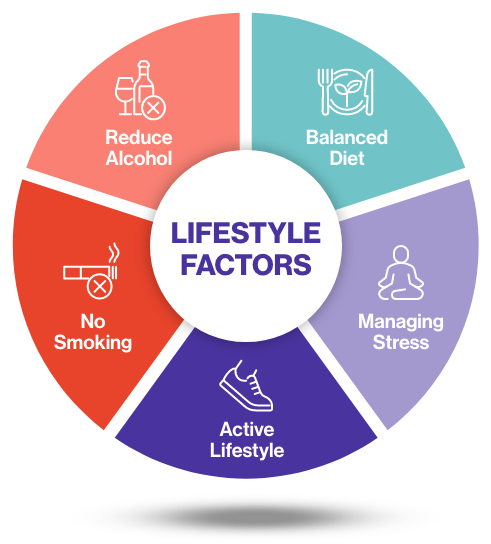
There are no guarantees against cancer. But there are things you can do to reduce your risk of breast cancer by making small, healthy changes in your life.
Maintaining a healthy lifestyle — including regular exercise, a balanced diet, stress management, quitting smoking, and reducing alcohol intake — may help lower the risk of recurrence, support your overall well-being, and help you through your treatment plan.23,24

While it’s impossible to eliminate the risk of cancer recurrence, there are several steps you can take together with your healthcare team to help reduce the risk of your cancer coming back:2
Chemotherapy - Chemotherapy is a standard treatment for some types of cancer. It uses anti-cancer drugs to destroy cancer cells. It is a systemic treatment which means it works throughout your body. Sometimes doctors use the word cytotoxic to describe the way chemotherapy works. Cytotoxic means toxic to cells.16
Whether chemotherapy is a suitable treatment for you, and which drugs you might have, depends on your type of cancer, what the cancer cells look like under a microscope, whether the cancer has spread and your general health.16
Targeted therapies - Targeted therapies are often used in combination with hormone therapy to target cancer cells that may have remained after surgery or other initial treatment to stop them from growing again.4
Radiotherapy - Radiotherapy means the use of radiation, usually x-rays, to treat cancer. You might have radiotherapy from inside the body, called internal radiotherapy. Or external radiotherapy, which is from outside the body. You may have radiotherapy to try to cure cancer, to reduce the chance of cancer coming back, or to help relieve symptoms.17
You might have it by itself or with other treatments, such as chemotherapy or surgery. Most types of radiotherapy use photons. But you might have electrons or more rarely protons. Your doctor decides which type you need.17
Hormone therapy - Also called endocrine therapy, this is the most common adjuvant treatment for HR+/HER2- breast cancer.5 patients will usually receive this for 5-10 years to reduce the risk of cancer recurrence.4,6
Immunotherapy - Immunotherapy uses our immune system to fight cancer. It works by helping the immune system recognise and attack cancer cells. You might have immunotherapy on its own or with other cancer treatments. Immunotherapy is a standard treatment for some types of cancer. You may hear some types of immunotherapy described as targeted or biological therapy.19
You should have regular conversations with your doctor about whether adjuvant therapy is a suitable option to help reduce the risk of your cancer returning and increase your chances of a cancer-free future.3
Even if you’re in remission, it’s important to stay vigilant for any potential signs of recurrence. Some red flag symptoms to watch out for include:7,8
Swelling or lump on your chest, breast, in your armpit or around your collarbone
A change in shape or size of your breast
A change in skin texture, such as puckering or dimpling
The nipple has become pulled in (inverted) or looks different, for example changed position or shape
Liquid (discharge) that comes from the nipple without squeezing it
Ongoing general feeling of being unwell e.g. tiredness, nausea, headaches, dizziness, unexplained weight loss
Redness or a rash on the skin, in or around the nipple or in the area of the mastectomy scar line of your treated breast
A lump or thickening that feels different (with your treated breast this could be on or away from the scar line)
Unexplained body pain, swelling or fluid retention
Unexplained speech, vision and/or memory problems
Breathlessness and/or persistent cough
If you notice any of these symptoms or anything else unusual, it’s crucial to report them to your doctor as soon as possible. The earlier you catch the symptoms; the sooner appropriate interventions can be taken.

Please fill in your answers below.

References:
UK | September 2025 | FA-11295732-2
Keep Ahead has been developed and funded by Novartis Pharmaceuticals UK Limited. It has been created in collaboration with primary breast cancer patients whose knowledge and insights have informed the content and direction for the campaign.
This website is part of a programme that is funded by Novartis Pharmaceuticals UK Limited. Novartis Pharmaceuticals UK Limited is a private limited liability company registered in England and Wales under number 119006. Registered office 2nd Floor, The WestWorks Building, White City Place, 195 Wood Lane, London, W12 7FQ. Use of this website is governed by our Terms of Use and the Cookies and Privacy Policy.
Reporting side-effects
If you get side effects with any medication you are taking, talk to your doctor, pharmacist or nurse. This includes any possible side effects not listed in the information leaflet that comes in the pack. You can report side effects via the Yellow Card Scheme at www.mhra.gov.uk/yellowcard. By reporting side effects, you can help provide more information on the safety of your medication.
© 2025 Novartis Pharmaceuticals UK Ltd - UK | May 2025 | FA-11340321-1. This site is intended for a UK early breast cancer patients and general public.
